Caring and ‘Help’
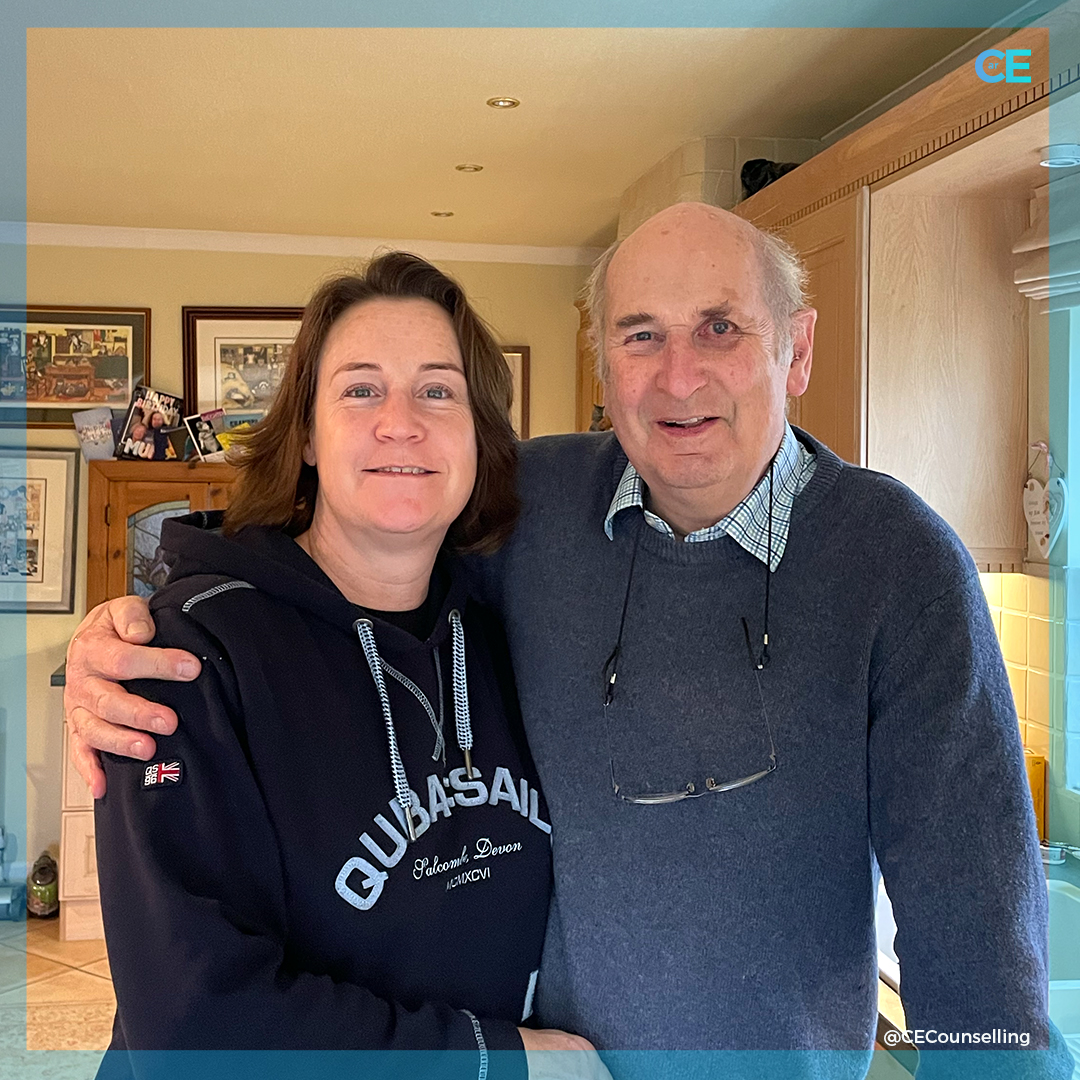
It is dark and as the sun slowly starts to rise, the song thrush sings from the distance. I am at my Dads’ house. Last night he called with the first middle of the night ‘help’. He was having heart issues which he felt were like a heart attack and he sounded scared. “I need some help with this” he stated as the Doctor in him rationalised what might be happening. I packed a bag, kissed my husband and drove 2 hours to be with him. When I arrived the Ambulance was just leaving with Dad not in it. He was well enough to not go to hospital but needed to see his GP the next day. As a non medic I questioned this but was assured by the amazing Ambulance crew that he was OK, for now. [Since writing this he has been checked by a Cardiologist and is OK still, for now]
Dad’s Fragility
This is the first time Dad has shared his fragility with me. He is 83 and has been caring for Mum for the last 10 years, she has Dementia. He is exhausted! It is so hard for anyone caring for a loved one as they are on call 24 hours a day and it is relentless. The despair of the future sits in the living grief and the isolation of their day to day demands often leaves carers lonely with a loss of their own joi de vive. The only true respite will come when the one they love dies and that is the not the respite they look forward to or want!
Caring for his Wife
Sitting in the sun room next to my incognisant Mum, I reflect on the stark reality of Dad’s life as he cares for Mum 24/7. I look at Mum and wonder if she even knows I am in the room, she rarely opens her eyes now and we do wonder how much vision is left behind what were once vibrant piercing blue eyes. Dad potters around the kitchen making protein smoothies with fresh fruit he bought from the shop this morning with his daily paper. He spoon feeds his wife so gently and calmly, wipes her face and makes sure she is still sitting upright. She is propped up on both sides as her muscles have weakened so much that she is no longer able to sit up without the support. It is so heartening and so utterly sad to see!! Dementia is a long, slow, cruel illness which affects not just the one with it but all those around. My Dad has lost his wife but he has also lost his freedom to live out their retirement together. He is isolated in his care giving and love to Mum. He never complains and I do wonder how much of the sadness I feel he hides beneath the veneer of his smile. I doubt I will ever know as Dad is a stoic and proud man.
Carers are the unsung heroes
Caring for a loved one is relentless, often thankless and usually exhausting. I have witnessed the way caring can take all the energy and light out of Dad and others I have worked with through counselling. Carers are the unsung heroes, the ones who keep on going because they have to, the ones who get forgotten in the midst of the illness of the one they are caring for.
Support for Carers
If you visit a loved one who is ill and being cared for please make time for the carer as it will be them who need your support, empathy, sympathy, time and conversation so much more I expect than the one they are caring for. Ask the carer if they are OK, if they want some respite, if there is anything you can do which will be of support for them. If you can spare a few hours, ask them if they want to go out and be free of their caring for a few hours whilst you cover for them. It is the little offerings which make a big difference to carers. Don’t lose sight of their needs in the fog of the illness of the one they are caring for. Also, in my experience, carers will be the last ones to ask for help but the first ones who need it to be offered!!
Massive Thank you
To finish this blog I want to say a massive thank you to Dad and all the wonderful people who go out of their way every day to make the lives of others better, richer, more comfortable and enable the ones who they care for to be OK for another day. They literally could not do it without you.
Take time when you can to take care of you too.
Written by your local counsellor in Fleet, Caroline at Caroline Ellison Counselling – this is my experience and these are my opinions. Carpe Diem.
Alzheimer’s and Dementia support
If you are an Alzheimer’s and Dementia carer, you are not alone, there are many people who are here to support you. There are helplines and support groups who will offer support, below are some of those who can offer expert advice. I specialise in Counselling for Carers and counselling for Alzheimer’s and Dementia and am here to support you.
After a diagnosis of dementia: next steps – This checklist has been written by dementia specialist Admiral Nurses, to help in the early days after you or your family member has received a diagnosis of dementia.
Website: Steps to take after diagnosis of Dementia
Alzheimer’s Society
Provides information on dementia, including factsheets and helplines.
Phone: 0333 150 3456 (Monday to Friday, 9am to 5pm and 10am to 4pm on weekends).
Website: www.alzheimers.org.uk
Talking Point, on-line dementia and their carers: foum.alzheimers.org.uk
Alzheimer’s Research UK
The leading dementia and Alzheimer’s disease research charity.
Phone: 0300 111 55555
Website: https://www.alzheimersresearchuk.org/
Alzheimer’s Association
Lots of information on their site with links. They strives to improve quality of life for those facing Alzheimer’s disease and other dementias.
Website: https://www.alz.org/uk/dementia-alzheimers-uk.asp
Alzheimer Café UK
Website UK: http://www.alzheimercafe.co.uk/
Website Farnborough: http://www.alzheimercafe.co.uk/Farnborough.htm
Carer’s allowance
If you’re caring for someone with dementia, you may be entitled to certain benefits. This page will tell you if you’re entitled to Carer’s allowance: https://www.alzheimers.org.uk/get-support/legal-financial/carers-allowance
Carer Support and Dementia Advice Service for Hampshire
Provides advice, information and support to all carers aged 18 and above who provide care for an adult. The service also supports people with dementia and memory problems and is available throughout Hampshire.
Phone: 01264 332297
Email: enquiries@andovermind.org.uk
Care Choices
Committed to helping people who need information on social care and support. Find the Care Home or Care Solution that’s best for you – get information, guidance and reviews. Phone: 01223 207770 Website: https://www.carechoices.co.uk/
Dementia Guidance
An independent dementia guide intended to provide a guide to free services available throughout the UK to people with dementia and their families.
https://www.dementiaguidance.co.uk
Dementia Friendly Hampshire
An independent charity, working to make Hampshire a county where people affected by dementia can live a good life.
Phone: 07388 668332
Email: jane.ward@dementiafriendlyhampshire.org.uk
https://dementiafriendlyhampshire.org.uk/
Dementia Friendly Hampshire – Advice and Information
This is a helpful list of things people who have dementia need to consider having in place.
Website: https://dementiafriendlyhampshire.org.uk/advice-and-info/
Dementia Talking Point – Alzheimer’s UK online community. Have you or someone you know been diagnosed with dementia? Join Dementia Talking Point to share experiences with other people affected by dementia.
Website: https://www.alzheimers.org.uk/get-support/dementia-talking-point-our-online-community
Find a Dementia Café or dementia service near you
Dementia Cafés offer a place to socialise, learn more about dementia and local services, and enjoy something new each session. Follow this link to find your local Café:
Website: https://www.alzheimers.org.uk/get-support/your-support-services/dementia-cafes
Alzheimer’s Drug Discovery Foundation
Website: https://www.alzdiscovery.org/
Brunel Care
Local Charity caring for older people across Bristol, South Gloucestershire, North Somerset and Somerset.
Phone: 0117 914 4200
Website: https://www.brunelcare.org.uk/
DEEP
DEEP stands for the Dementia Engagement and Empowerment Project – it is the UK network of dementia voices. DEEP consists of around 100 groups of people with dementia – groups that want to change things.
Contact Rachel Niblock – UK Coordinator for DEEP network.
Email: niblock@myid.org.uk
Phone: 07720 538851
Website: https://www.dementiavoices.org.uk/
Dementia Action Alliance
Support national and local for dementia support
Website: https://www.dementiaaction.org.uk/ / https://nationaldementiaaction.org.uk/
Dementia Adventure
Charity supporting people with dementia to get outdoors, connect with nature, themselves and their community, and retain a sense of adventure in their lives.
Phone: 01245 237548
Email: info@dementiaadventure.co.uk
Website: http://www.dementiaadventure.com/
Dementia Connect Helpline
Phone: 0333 150 3456
Wales and West Midlands
Dementia UK
Telephone or email advice and support for family carers, people with dementia and professionals provided by experienced Admiral nurses.
Phone: 0800 888 6678
Website: www.dementiauk.org
Royal Airforces Dementia Support
Phone: 0800 018 2361
Email: dementia@rafa.org.uk
Website: https://dementia.rafa.org.uk/
NHS Information
An overview of Alzheimer’s disease. Signs and symptoms of Alzheimer’ disease
Website: https://www.nhs.uk/conditions/alzheimers-disease/
Play List for Life
Charity founded by Sally Magnusson after death of her mother who had dementia. Music for everyone living with dementia which can make it easier and happier
Phone: 0141 404 0683
Email: info@playlistforlife.org.uk
Website: https://www.playlistforlife.org.uk/
The Wide Spectrum
Dementia education resources
Website: http://www.thewidespectrum.co.uk/default.htm
Young Dementia UK
Support for those with early onset dementia. Young Dementia UK have teamed up with Dementia UK.
Dementia Helpline UK: 0800 888 6678
Website: https://www.youngdementiauk.org/
Counselling Directory – https://www.counselling-directory.org.uk/dementia.html
This list is by no means comprehensive so if you know of other support available I will be very grateful if you will let me know so that I can add them to the list for others to find. Email me please. carolineellisoncounselling@gmail.com